Fall detection in the elderly
Falls are a major public health problem in the elderly and is a leading cause of unintentional injury and deaths in the elderly population worldwide. A fall episode can have profound implications on their independence, health and overall quality of living, imposing additional socio-economic burdens. Many complications from an unattended fall could be prevented if prompt help was received or properly detected in situations of daily life. Over the years many fall detection devices have been proposed for the elderly, but many do not provide an effective solution. The most promising angle of fall detection seems to be the use of accelerometers. However, there are many different approaches on placement of accelerometers for fall detection, and it seems uncertain which one is preferable. Generally, there are a few evaluation criteria and consideration factors.
Criteria of fall detection systems
The placement site can largely affect the four possible situations of a fall detection system (Noury, N., et al.):
- true positive (TP), a fall occurs and the system correctly detects it;
- false positive (FP), the system declares a fall event, but it did not occur;
- true negative (TN), a normal fall-like movement is performed, the device does not declare a fall;
- false negative (FN), a fall occurs, but the system does not detect it.
Three criteria are proposed to evaluate the reliability of a fall detection system (Abbate S., et al.):
- sensitivity = TP/(TP + FN), the ability to detect all real falls;
- specificity = TN/(TN + FP), the ability to detect only real falls;
- accuracy = (TP + TN) /(TP + FP + FN + TN), which is the proportion of true results in the considered data set
Aside from the capacity of the fall detection system, usability is also often considered as it is a fundamental factor for real adoption of a fall detection system.
Review of accelerometer placement strategies
A brief review on promising accelerometer placement strategies in present literature was performed by a current student from Maastricht University as part of Masters coursework. Three studies stood out when validity was compared based on three attributes: sensitivity, specificity and usability.
Study #1 (Kangas M., et al.)
The first study used three sensors (forehead, waist and wrist), which achieved a specificity and sensitivity of 100% and 98% respectively. When the data gathered by the wrist sensor was excluded, reliability was only slightly lower. Despite a high validity, the placement of a sensor on the forehead makes this an undesirable option for use in daily life.
Study #2 (Gjoreski H., et al.)
The second study used four sensors (sternum, waist, thigh and ankle; and found a specificity and sensitivity of 99% and 97.8% respectively. This sensor placement would probably be preferable to the one used by Kangas as it is less obtrusive. However, it would require regular replacement of four sensors which likely lead to low compliance, hence defeats the purpose of using this placement strategy for accurate fall detection.
Study #3 (Abbate S., et al.)
Lastly, the third fall detection system included a smartphone-based setup. It was found that data from a single sensor on the thigh analysed by the smartphone, in conjunction with the smartphone’s integral accelerometer, achieved a specificity of 100% but a relatively low sensitivity of 96.3%. When using only the smartphones integral sensor without an additional sensor, both sensitivity and specificity were too low to qualify as accurate fall detection. The disadvantage of using the smartphone for fall detection in the study is the need to be carried (within range of 3 meters) and to remain charged at all times. This is not always feasible. Furthermore, carrying a smartphone enables the individual to contact relatives or caregivers for assistance in the event of emergency if a fall should happen. In this context, the possibility of using a small external sensing unit can greatly reduce the intrusiveness of the system.
Conclusion
The author concluded that there is currently no clear optimal placement that will outperform the others in every situation. For home use, the smartphone based setup would likely have the populations’ preference, although there is a high chance of the phone being out of reach when it is most needed, when compared to accelerometer-only setups. For research purposes the placements used by Kangas and Gjoreski would have the upper hand based on sensitivity, although gathering subjects for field research may be easier when only one sensor and a Smartphone are required.
Comments
The proposed placement strategies and accelerometers for fall detection in the elderly are numerous, and reliability may be comparable. However, fall detection systems based on wearable sensors are reliant on user compliance (remembering to wear the device and choosing to wear the device). Therefore, it is expected that systems with multiple sensors will be less favourable and result in lower compliance in the elderly.
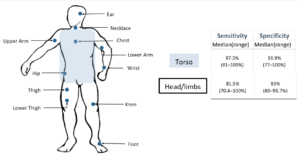
Fall detection systems with single sensors placed on the torso is the most common, as revealed revealed in a systematic review (Chaudhuri et al., 2014). Illustration on the right shows the sensitivity and specificity of such systems with respect to the sensor location. Devices placed on the torso had a sensitivity and specificity with a median sensitivity and specificity of 97.5% (81–100%) and 96.9% (77–100%) respectively (Chaudhuri et al., 2014). Whereas, devices placed around the head and limbs had a lower median sensitivity and specificity of 81.5% (70.4–100%) and 83% (80–95.7%) respectively. Those involving multiple sensors had a median sensitivity of 93.4% (range 92.5–94.2) and a median specificity of 99.8% (range of 99.3–100).
Although many fall detection systems show high sensitivity and specificity in simulated research settings, it is important to take note that it may not reflect the same reliability in real-world situations. As algorithms are optimized to the test situation, real-world tests would be a more rigorous indicator of the device’s reliability. However, few have been performed. Therefore, more real-world tests may be necessary to prove the efficiency of these systems before implementing it as a feasible solution for fall detection in the elderly.
References
Abbate S, Avvenuti M, Bonatesta F, Cola G, Corsini P, et al. A smartphone-based fall detection system. Pervasive and Mobile Computing. Vol 8 (6). Dec 2012.
Gjoreski H, Lustrek M, Gams M. Accelerometer Placement for Posture Recognition and Fall Detection. Intelligent Environments. 2011.
Kangas M, Konttila A, Lindgren P, Winblad I, Jamsa T, et al. Comparison of low-complexity fall detection algorithms for body attached accelerometers. Gait & Posture. Vol 28 (2). Aug 2008.
Noury, N., Rumeau, P., Bourke, A. K., ÓLaighin, G., & Lundy, J. E. (2008). A proposal for the classification and evaluation of fall detectors. Irbm, 29(6), 340-349
Acknowledgements
The review of accelerometer placements in the current literature was contributed by Gerard van der Linden, a current Masters student in Maastricht University’s Faculty of Health, Medicine and Life Sciences (FHML).
for more information about MOX Accelerometry or fall detection algorithms.